Your next DNA vaccine might come from tobacco
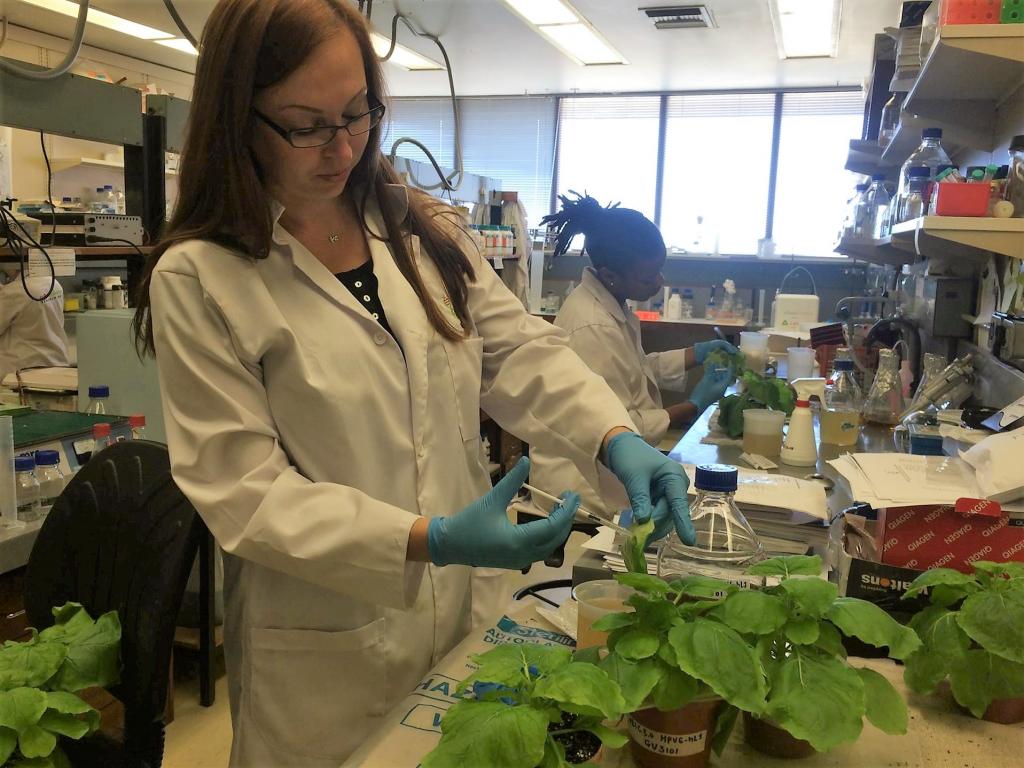

Dr Anne Meyers, Professor Ed Rybicki and Dr Inga Hitzeroth of the Biopharming Research Unit, seen here with young tobacco plants. Image credit: BRU
“We’ve succeeded in making a completely mammalian viral particle in a plant - proteins, DNA, everything. That’s enormously exciting,” says Dr Inga Hitzeroth of the Biopharming Research Unit (BRU) at UCT.
In an Open Access study just published in Nature Scientific Reports, BRU researchers report using tobacco plants to create a synthetic viral particle known as a pseudovirion. A pseudovirion looks like a virus, but it contains no infectious viral DNA. A virus is usually made up of a shell surrounding the virus’s own genetic material. Pseudovirions instead carry whatever DNA the researcher wishes to include within the shell of proteins that make up the outer coating of the virus. Until now, such particles have only ever been created in yeast or mammalian cell cultures - this is the first time researchers have successfully created pseudovirions in plants.
The BRU is part of a new movement known as biopharming, which means using plants as biological factories. Biopharming has been used to create flu vaccines, potential Ebola drugs, and an enzyme used to treat Gaucher’s Disease in humans. The technique employs the cellular machinery within tobacco plants or other plant cells to manufacture enzymes, antibodies or even the viral capsid proteins (the proteins that make up the shell of a virus), which act as vaccines. In this research, the BRU has taken biopharming one step further by using plants to create a viral shell that encloses ‘custom’ DNA selected by researchers. “What’s unique here is that DNA that was manufactured within the tobacco plant is now being incorporated into a viral particle to form a pseudovirion,” says Hitzeroth. The shell of this pseudovirion was that of human papillomavirus (HPV) type 16, the virus responsible for over 50% of cervical cancer cases worldwide. The The BRU team hope this new plant-based technology could one day be used to test future HPV vaccines. First author of the study, Dr Renate Lamprecht, explains: “We need pseudovirions to test any new HPV vaccine candidates. At the moment it is very expensive to make pseudovirions – we need to make them in mammalian cell culture, it needs to be sterile, and the reagents are very expensive.”
All these factors contribute to the high cost of current HPV vaccines, which are actually virus-like particles. Virus-like particles (VLPs) are similar to pseudovirions, but they contain no DNA. Plant-made pseudovirions, as demonstrated by this study, could reduce the cost of testing and manufacturing such vaccines, thus helping to make HPV vaccines affordable where they are needed most: the developing world.
The BRU team compared these new plant-made pseudovirions against the more widely-used mammalian cell culture-produced particles by using what’s known as a neutralisation assay. In this test (which is commonly used to test new HPV vaccine candidates), cells are ‘infected’ with pseudovirions, with or without pre-treatment with neutralising antibodies. The DNA inside the pseudovirion carries a ‘reporter gene’ that produces a protein that can give off a light signal. Thus, an infectious pseudovirion gets into the cell and gives off light, but one that is stopped by neutralising antibodies does not.
“I was jumping up and down the first time I saw the neutralisation results, but I repeated the experiment a few times to be sure, asking myself, ‘is everything correct, are all the controls there?’” explains Lamprecht. “It was a very exciting moment for us when we confirmed that neutralisation had occurred.”
Right now, every laboratory makes pseudovirions for such neutralisation experiments themselves. Dr Hitzeroth hopes that one day, they won’t have to: “we’re in the initial stages, but if we optimise the process and get the yield much higher, we think it’s a product that could be sold all over the world.”
Dr Renate Lamprecht and Sandiswa Mbewana prepare tobacco plants to produce pseudovirions. Image credit: BRU
For Professor Ed Rybicki, Director of the BRU, this achievement was enormously satisfying, as it brought together two strands of his research interests that have co-existed for over 20 years. “Seventeen years ago, I had the idea to combine making HPV VLPs in plants with a DNA plant virus we were working on, to see if we could make pseudovirions. It took until now for the technology to finally come together, but it shows what can happen in biotechnology if you’re willing to persevere.”
The BRU are also hoping to use this technology to create a therapeutic vaccine, which would also be a first of its kind. The idea would be to use the pseudovirion to deliver DNA that could treat an ongoing HPV infection or even a tumour. With global acceptance and support for the biopharming movement growing rapidly, it might not be too long before the first plant-produced HPV vaccine is making a difference in Africa and around the world.
